Cervical cancer

Cervical cancer is a disease that can be prevented and cured when diagnosed in time. Over 80% of women in whom cancer was diagnosed at an early stage are fully cured. Cervical cancer is the most common cause of cancer death in women in developing countries and the second largest cancer, after breast cancer, in women worldwide. In Greece, around 1,000 women each year develop cervical and endometrial cancer·
most of them had never had a Pap test.
The uterus is the organ in which the fetus develops and holds during pregnancy. In the lower part of the uterus there is a narrow passage 2-3 cm long that forms the cervix and is located exactly where the vagina ends.
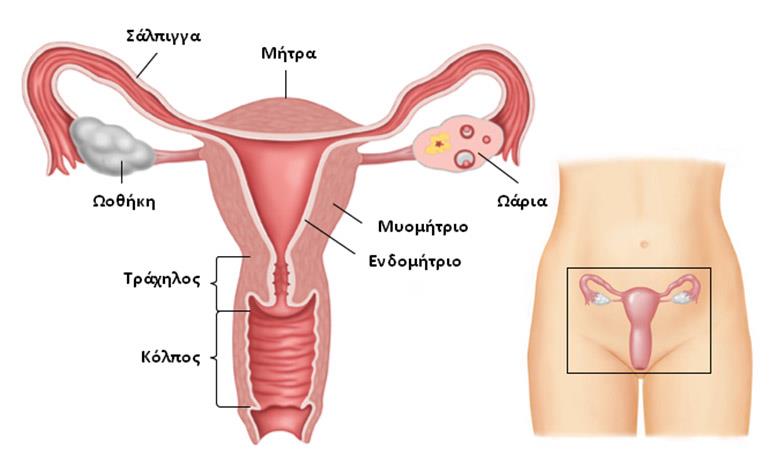
Typically, tumors that grow in this area start in the so-called transition zone. This is an area where the inner part of the cervix (endocervix) meets, which is closer to the body of the uterus, with the outer part of the cervix (extracervical), ie where the vagina meets the cervix. Cervical cancer usually grows slowly for many years. Before cancer develops, changes in the tissues of the area occur at the cellular level (called malformations or precancerous lesions). It is very important to know that in this early precancerous stage, these dysplastic cells can be eliminated with simple therapeutic interventions.
In the past, cervical cancer was one of the most serious gynecological cancers. Today, however, thanks to the early diagnosis with the Pap test, the vast majority of women who will be diagnosed early, will be cured of the disease.
Causal Factors
The most important risk factor for developing cervical cancer is human papilloma virus (HPV) infection, which is transmitted through sexual intercourse, even if it is not complete. Using a condom does not provide complete protection.
The most common subtypes of the virus are 16 and 18. For at least 2 decades, the HPV virus has been known to cause cervical cell dysplasia and other precancerous lesions, which can develop into cancer if left untreated.
Other risk factors are:

It should also be noted that patients with a weakened immune system (eg patients with AIDS, or immunosuppressed) are at risk of developing cervical cancer.
Prevention
Evidence that HPV infection is the most important risk factor for developing cervical cancer has led to scientific research into a vaccine that protects against the HPV subtypes 6, 11, 16 and 18 that are responsible for 80 % of cervical cancers.
Vaccination is recommended for girls and young women aged 9-26 years before sexual intercourse. It is included in the National Vaccination Program and is given free of charge to all girls 12-15 years old along with other pediatric vaccines, but also to adolescent and young women 16-26 years old who did not have time to be vaccinated at the age of 12-15 years. It should be emphasized that the vaccination does not protect against all subtypes of the HPV virus and does not involve a change in the current guidelines for gynecological examination and Pap smear per year, since in this way the possible lesions are diagnosed and treated in time. It is also recalled that the use of a condom is mandatory not only against HPV but also other sexually transmitted diseases.
Vaccination and regular Pap tests now provide the best possible protection against cervical cancer.
The Pap test is a simple, painless and bloodless test. It is done after the beginning of the woman's sexual activity, between the 10th and 20th day of the cycle, and at a frequency determined by the doctor.
Covered by all insurance funds.
Symptoms
In the early stages, cervical cancer is often asymptomatic. For this reason, it is very important to visit the gynecologist regularly (at least once a year) for a Pap test. When the disease is more advanced the following symptoms may be present and immediate medical evaluation is needed:
CAUTION: the above symptoms can be due to various causes and do not necessarily indicate the presence of malignancy. The basic rule is that they should be examined immediately by the gynecologist.
Diagnosis
The Pap test is the easiest method to detect dysplastic lesions and precancerous lesions that can lead to the development of cervical cancer, if not treated.

Treatment
Treatment options depend mainly on the stage of the disease (tumor size, infiltration depth, spread of the disease to neighboring or other organs of the body). Therapeutic methods include:

